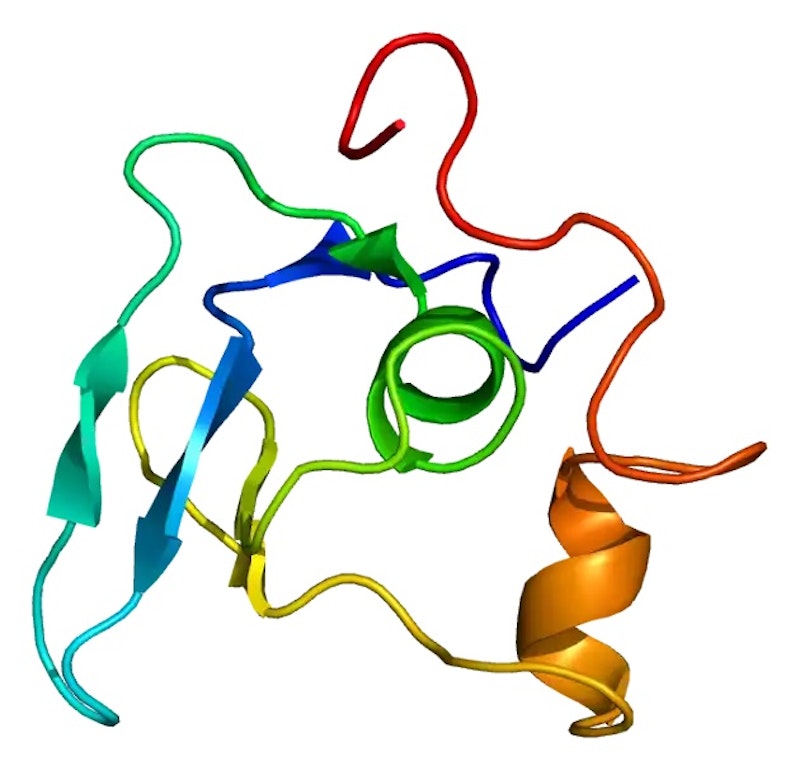
Readers of my previous installment might wonder how and/or why my ascending aorta needed replacing. The aorta’s the fat blood vessel that departs the left ventricle via the aortic valve, feeding fresh blood to the body. The failure in my aorta was due to a deformity on a gene that produces a protein that codes for connective tissue. The protein is elastin, which makes up cells that can expand and contract as needed. The gene is FBN-1 and is found on Chromosome 15. It has hundreds of variants.
Connective tissue is the material that holds most body parts in place. Failure of this tissue might cause the pupils of the eyes to drift out of place; it might cause the body to be exceptionally long and thin, with the arm-to-arm wingspan exceeding the person’s height. It might cause extremely loose joints, or a caved-in sternum. I once met a patient who could clasp her fingers together behind her back. This combination of symptoms is called Marfan’s Syndrome, named in 1896 after Dr. Antoine Marfan. It’s not a disease, but more accurately a collection of problems. These patients sometimes refer to themselves as Marfs, and one needs three of the “problems” to qualify. Technically, I’m not a Marf.
The aorta’s made up of three layers, one inside another. In cases such as mine, the middle layer, or media, was adversely affected by an FBN-1mutation, causing the aorta to lose its elasticity; it just keeps dilating until it bursts or is repaired. This is called cystic medial necrosis. If you have an issue with the FBN-1 gene, that middle layer eventually gives out. My mother was 71, my brother was 35, I was 50; the youngest patient I ever met had surgery at nine.
I didn’t know any of the physiology until I passed out on the basketball court one day and ended up in the hospital. This was near Boston. They found that I was in atrial fibrillation, that my ascending aorta was half again the diameter of normal, and that my aortic valve had two leaflets instead of three, and was leaking. They described an “insufficiency” in the mechanism by which the heart transmits blood, oxygen really, where it needed to be.
When blood departs the left ventricle, it does so under great pressure, normal being around 120mm mercury (hg). This is the higher (systolic) number of your blood pressure reading, and it’s this pressure that beats the hell out of the first few inches of the ascending aorta. When the heart pumps, the aorta expands; its recoil helps drive the blood forward. The leaky aortic valve allows some of this blood to flow backwards, which makes the left ventricle work harder.
Three-quarters of people with this FBN-1 disorder are born that way; I inherited mine from my mother, who died when her aorta gave out. The other cases represent spontaneous mutations of the gene. There’s no cure; they try to slow the dilation down with drugs like beta blockers and calcium channel blockers, which weaken the force of the heart’s contractions. My aorta continued to grow long after adulthood, and it took 10 years before I required preventative surgery. During those years, doctors monitored the enlargement, called an aortic aneurysm, with all kinds of exotic imaging machines: gamma cameras, x-rays, CT chance, echocardiography, MRI.
The final exam comes the day before surgery, and Involves taking pictures of the blood vessels; it’s called angiography. I was sent to the cardiac cauterization lab; there, they checked my coronary arteries to make sure there would be no surprises when the cut me open, such as clogged arteries. They inject contrast dye into the coronaries, to look for blockages. I was awake for this. The arteries fill with contrast and turn black; they look like tree roots. One or two heart beats later, the dye is flushed away. It seemed like magic. This was the beginning of my infatuation with cardiology.
Two years of study later, I took a job in the cath lab. It was the most interesting work I ever had.